Diabetes mellitus is a metabolic disorder that has the risk of complications in multiple organs, such as the heart, kidneys, and eyes, as well as complications in multiple connective tissues, such as bone, cartilage, and nerves. There is a variety of connective tissues in the spine that may be adversely impacted by diabetes. This page reviews several common back pain conditions that are thought to be linked to diabetes.
In This Article:
- Uncontrolled Diabetes Linked to Chronic Back Pain
- Types of Back Problems Linked to Diabetes
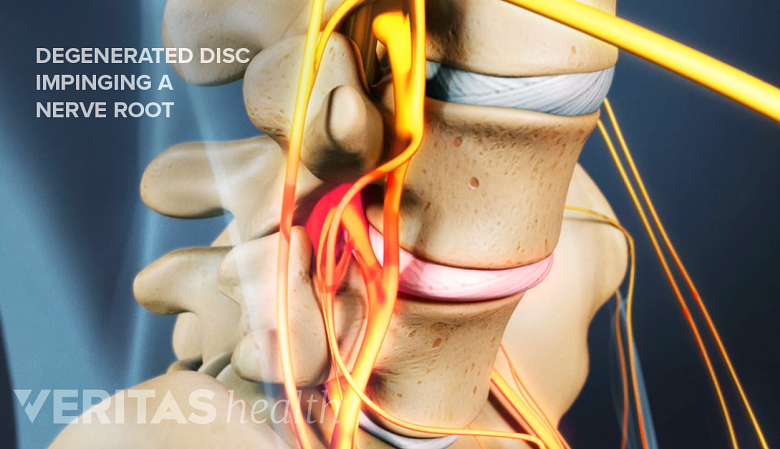
Lumbar Disc Degeneration
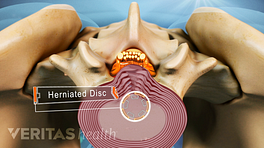
Prolonged uncontrolled diabetes increases the risk of lumbar degenerative disc disease.
Lumbar disc degeneration is characterized by back pain caused by the breakdown of one or more the spinal discs in the lower back.
See Lumbar Degenerative Disc Disease (DDD)
After more than 10 years of living with diabetes, individuals are at greater risk of developing painful disc degeneration in the lumbar spine (lower back). If the diabetes remains uncontrolled for that duration of time, the increased risk for lumbar degenerative disc disease is compounded further. 1 Liu X, Pan F, Ba Z, Wang S, Wu D. The potential effect of type 2 diabetes mellitus on lumbar disc degeneration: a retrospective single-center study. J Orthop Surg Res. 2018;13(1):52. Published 2018 Mar 14. doi:10.1186/s13018-018-0755-8 Keeping diabetes under control may be critical for preventing or delaying the toll of disc degeneration on the lower back.
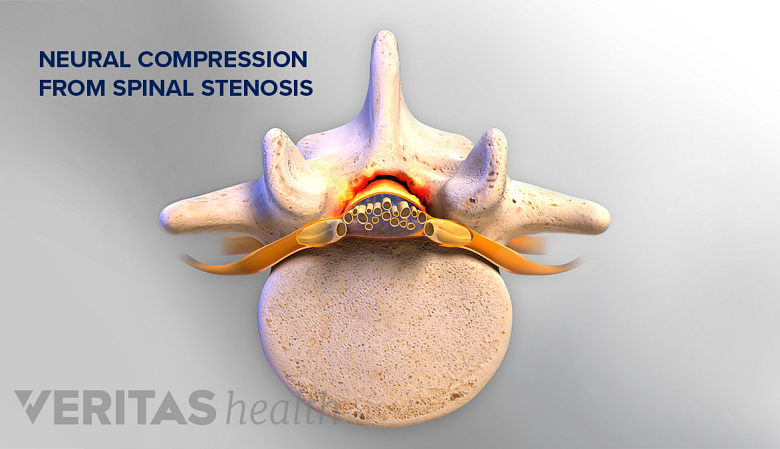
Spinal Stenosis
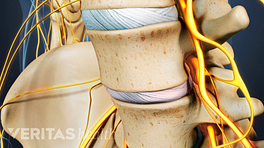
Diabetes may be associated with the development of spinal stenosis.
Spinal stenosis is a narrowing of the bony openings (foramina) of the spine, which leaves less space for the exiting spinal nerves.
Diabetes may be associated with the development of spinal stenosis, particularly in the lumbar region of the spine. Up to 25% of patients with lumbar spinal stenosis were found to have diabetes and/or high blood pressure, according to one study. 2 Anekstein Y, Smorgick Y, Lotan R, et al. Diabetes mellitus as a risk factor for the development of lumbar spinal stenosis. Isr Med Assoc J. 2010;12(1):16-20. Another study found that this connection may be stronger in women; around 36% of women with lumbar spinal stenosis were found to have diabetes. 3 Asadian L, Haddadi K, Aarabi M, Zare A. Diabetes Mellitus, a New Risk Factor for Lumbar Spinal Stenosis: A Case-Control Study. Clin Med Insights Endocrinol Diabetes. 2016;9:1-5. Published 2016 May 5. doi:10.4137/CMED.S39035
See Spinal Stenosis Symptoms and Diagnosis
Vertebral Osteomyelitis
Vertebral osteomyelitis is usually caused by a bacterial infection, usually from Staphylococcus aureus, which can start in the vertebral bone and spread to the spinal disc.
See Osteomyelitis, a Spinal Infection
Diabetes increases susceptibility to infection and vertebral osteomyelitis. For example, an infected ulcer in a diabetic patient’s foot may be accompanied by lower back pain and a fever. Such symptoms may be related to vertebral osteomyelitis. 4 Mantovani A, Trombetta M, Imbriaco C, et al. Diabetic foot complicated by vertebral osteomyelitis and epidural abscess. Endocrinol Diabetes Metab Case Rep. 2016;2016:150132. doi:10.1530/EDM-15-0132
Spinal Epidural Abscess
Spinal epidural abscess refers to a rare infection that can start in the area between the vertebral bones and the membrane of the spinal cord.
Because diabetes increases the risk of infection, it also raises the risk of epidural abscess. Diabetes-related factors, such as obesity and hypertension, also increase the chance of infection. The risk of an abscess may increase even further with viral infections, including COVID-19. 5 Talamonti G, Colistra D, Crisà F, Cenzato M, Giorgi P, D'Aliberti G. Spinal epidural abscess in COVID-19 patients. J Neurol. 2021;268(7):2320-2326. doi:10.1007/s00415-020-10211-z
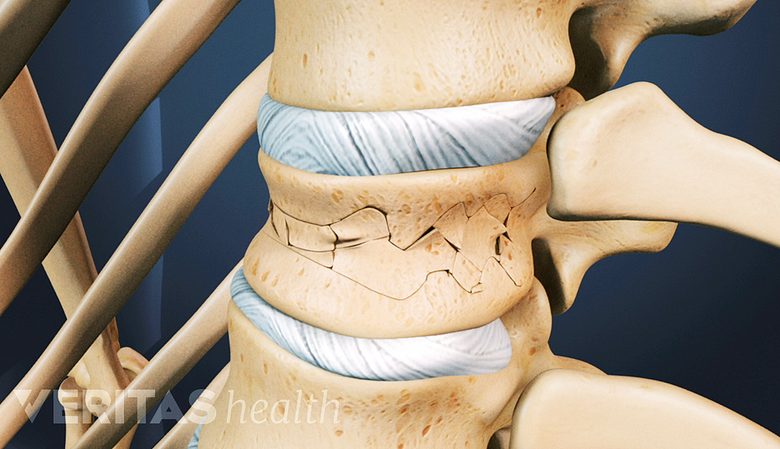
Vertebral Fracture (Osteoporotic Fracture)
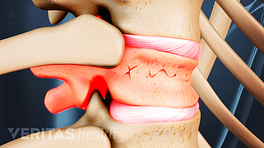
Diabetes reduces bone minerals, raising the risk of fractures in the vertebral bones.
A vertebral fracture related to osteoporosis, also known as an osteoporotic fracture or a compression fracture, is a type of break in the vertebral bone—the bony building blocks of the spinal column.
See When Back Pain Is a Spine Compression Fracture
Diabetes may alter the amount of minerals in the bones, making the bones more fragile and increasing the risk of a fracture. 6 Poiana C, Capatina C. Fracture Risk Assessment in Patients With Diabetes Mellitus. J Clin Densitom. 2017;20(3):432-443. doi:10.1016/j.jocd.2017.06.011 While well-controlled diabetes may pose less risk of sustaining a vertebral fracture, certain glucose-lowering medications (such as insulin, sulphonylureas, or thiazolidinediones) are associated with decreased quality and strength of the bones. 6 Poiana C, Capatina C. Fracture Risk Assessment in Patients With Diabetes Mellitus. J Clin Densitom. 2017;20(3):432-443. doi:10.1016/j.jocd.2017.06.011 , 7 Kalaitzoglou E, Fowlkes JL, Popescu I, Thrailkill KM. Diabetes pharmacotherapy and effects on the musculoskeletal system. Diabetes Metab Res Rev. 2019;35(2):e3100. doi:10.1002/dmrr.3100 , 8 Hidayat K, Du X, Wu MJ, Shi BM. The use of metformin, insulin, sulphonylureas, and thiazolidinediones and the risk of fracture: Systematic review and meta-analysis of observational studies. Obes Rev. 2019;20(10):1494-1503. doi:10.1111/obr.12885 An individual’s risk of fracture is assessed using diagnostic tools, and a physician can determine if these medications are to be avoided.
Neuropathic Pain
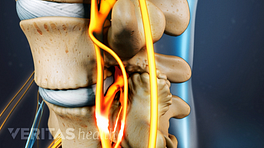
Neuropathy, or neuropathic pain, refers to a type of pain or weakness that originates in damaged nerves. Causes of such nerve damage may include injury, trauma, infection, or related conditions such as diabetes or regional pain syndrome.
See All About Neuropathy And Chronic Back Pain
Diabetic peripheral neuropathy occurs in the peripheral nerves, most commonly in the hands and feet. Nearly half of all people with diabetes experience diabetic peripheral neuropathy, 9 Iqbal Z, Azmi S, Yadav R, et al. Diabetic Peripheral Neuropathy: Epidemiology, Diagnosis, and Pharmacotherapy. Clin Ther. 2018;40(6):828-849. doi:10.1016/j.clinthera.2018.04.001 while neuropathic pain affects no more than an estimated 10% of the general population. 10 van Hecke O, Austin SK, Khan RA, Smith BH, Torrance N. Neuropathic pain in the general population: a systematic review of epidemiological studies [published correction appears in Pain. 2014 Sep;155(9):1907]. Pain. 2014;155(4):654-662. doi:10.1016/j.pain.2013.11.013 Adequate management of glucose levels is the primary treatment for diabetic peripheral neuropathy.
See Understanding Neuropathy Symptoms
For anyone with both diabetes and back pain or related symptoms, a coordinated approach for managing both the diabetes and the pain may be advisable.
- 1 Liu X, Pan F, Ba Z, Wang S, Wu D. The potential effect of type 2 diabetes mellitus on lumbar disc degeneration: a retrospective single-center study. J Orthop Surg Res. 2018;13(1):52. Published 2018 Mar 14. doi:10.1186/s13018-018-0755-8
- 2 Anekstein Y, Smorgick Y, Lotan R, et al. Diabetes mellitus as a risk factor for the development of lumbar spinal stenosis. Isr Med Assoc J. 2010;12(1):16-20.
- 3 Asadian L, Haddadi K, Aarabi M, Zare A. Diabetes Mellitus, a New Risk Factor for Lumbar Spinal Stenosis: A Case-Control Study. Clin Med Insights Endocrinol Diabetes. 2016;9:1-5. Published 2016 May 5. doi:10.4137/CMED.S39035
- 4 Mantovani A, Trombetta M, Imbriaco C, et al. Diabetic foot complicated by vertebral osteomyelitis and epidural abscess. Endocrinol Diabetes Metab Case Rep. 2016;2016:150132. doi:10.1530/EDM-15-0132
- 5 Talamonti G, Colistra D, Crisà F, Cenzato M, Giorgi P, D'Aliberti G. Spinal epidural abscess in COVID-19 patients. J Neurol. 2021;268(7):2320-2326. doi:10.1007/s00415-020-10211-z
- 6 Poiana C, Capatina C. Fracture Risk Assessment in Patients With Diabetes Mellitus. J Clin Densitom. 2017;20(3):432-443. doi:10.1016/j.jocd.2017.06.011
- 7 Kalaitzoglou E, Fowlkes JL, Popescu I, Thrailkill KM. Diabetes pharmacotherapy and effects on the musculoskeletal system. Diabetes Metab Res Rev. 2019;35(2):e3100. doi:10.1002/dmrr.3100
- 8 Hidayat K, Du X, Wu MJ, Shi BM. The use of metformin, insulin, sulphonylureas, and thiazolidinediones and the risk of fracture: Systematic review and meta-analysis of observational studies. Obes Rev. 2019;20(10):1494-1503. doi:10.1111/obr.12885
- 9 Iqbal Z, Azmi S, Yadav R, et al. Diabetic Peripheral Neuropathy: Epidemiology, Diagnosis, and Pharmacotherapy. Clin Ther. 2018;40(6):828-849. doi:10.1016/j.clinthera.2018.04.001
- 10 van Hecke O, Austin SK, Khan RA, Smith BH, Torrance N. Neuropathic pain in the general population: a systematic review of epidemiological studies [published correction appears in Pain. 2014 Sep;155(9):1907]. Pain. 2014;155(4):654-662. doi:10.1016/j.pain.2013.11.013