The steroids in epidural injections have anti-inflammatory effects that suppress pain signals from inflamed spinal nerves and improve function in the lower back and/or legs. 1 Manchikanti L, Kaye AD, Manchikanti K, Boswell M, Pampati V, Hirsch J. Efficacy of Epidural Injections in the Treatment of Lumbar Central Spinal Stenosis; A Systematic Review. Anesthesiology and Pain Medicine. 2015;5(1). doi:10.5812/aapm.23139
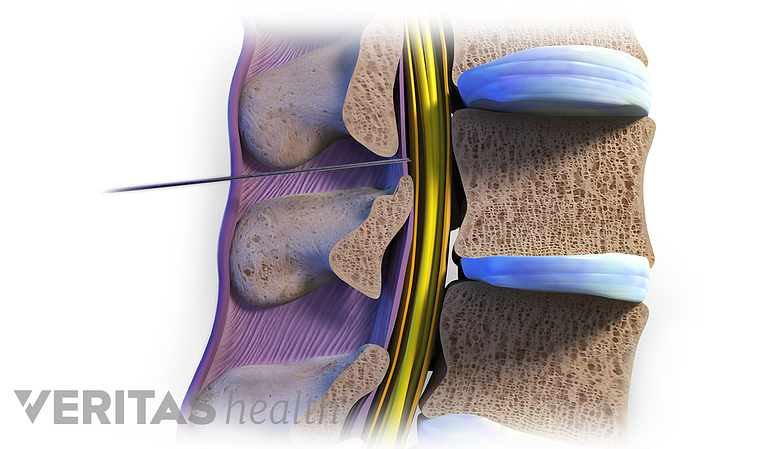
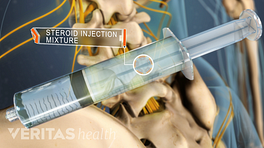
The medicated solution is injected directly into the epidural space. This space measures 3 to 6 mm 2 Manchikanti L, Kaye AD, Falco FJE, Hirsch JA. Essentials of Interventional Techniques in Managing Chronic Pain. Cham, Switzerland: Springer; 2018. and consists of the spinal nerves, dural sac (outer covering of the spinal cord), connective tissue, fat, and blood vessels. 3 Patel K, Upadhyayula S. Epidural Steroid Injections. [Updated 2019 May 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470189/
In This Article:
- Lumbar Epidural Steroid Injections for Low Back Pain and Sciatica
- How Epidural Steroid Injections Work
- Indications for Lumbar Epidural Injections
- Epidural Injection Procedure
- Epidural Steroid Injection Pain Relief Success Rates
- Epidural Steroid Injections: Risks and Side Effects
- Epidural Steroid Injections for Back Pain and Leg Pain Video
How Epidural Steroid Injections Control Inflammation and Relieve Spinal Pain
An epidural steroid injection may help control spinal nerve inflammation and pain.
Injected steroids control the inflammatory cascade induced by chemical, mechanical, and/or immunological irritants in the spine through the following mechanisms 4 Chang, Douglas, Zlomislic, Vinko. Chapter 273. Lumbar Spinal Injections. In: Chapman, Michael W. Chapman's Orthopaedic Surgery. Philadelphia: Lippincott Williams & Wilkins. https://www.researchgate.net/publication/327034223_Lumbar_spinal_injections_Chapman's_Orthopaedic_Surgery_Chapter_273. Accessed June 26, 2019. :
- Inhibit the release of chemical substances from discs. Chemical substances, such as phospholipase A2, may be released from degenerated or herniated intervertebral discs, which activate nerve fibers, causing pain. Steroids help synthesize specific inhibitors to stop the release of these chemicals.
- Limit the production of inflammatory mediators of pain. Steroids may limit the production of inflammatory pain mediators (proteins and other substances), such as leukotrienes and prostaglandins.
- Reduce spontaneous nerve pain signals. Steroids help suppress ongoing nerve pain by reducing spontaneous nerve signals originating from inflamed, irritated, or compressed nerves.
The effects of these injections are usually temporary, and progress in physical therapy and rehabilitation, as well as possible future injections may be recommended to provide long-term results. 3 Patel K, Upadhyayula S. Epidural Steroid Injections. [Updated 2019 May 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470189/
Types of Steroids Used in Epidural Steroid Injections
Steroids used in epidural injections differ based on particle size, solubility in water, and tendency to aggregate.
The steroids used in epidural injections differ based on their particle size, ability to dissolve in water, and aggregate or lump together.
Particulate steroids
Non-water-soluble steroids or particulate steroids have large particles. These particles may aggregate together and deposit at the site of nerve inflammation or compression for a long duration, providing long-term pain relief. Triamcinolone and methylprednisolone are examples of particulate steroids. 4 Chang, Douglas, Zlomislic, Vinko. Chapter 273. Lumbar Spinal Injections. In: Chapman, Michael W. Chapman's Orthopaedic Surgery. Philadelphia: Lippincott Williams & Wilkins. https://www.researchgate.net/publication/327034223_Lumbar_spinal_injections_Chapman's_Orthopaedic_Surgery_Chapter_273. Accessed June 26, 2019. , 5 Hassan KZ, Sherman Al. Epidural Steroids. [Updated 2019 May 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-.Available from: https://www.ncbi.nlm.nih.gov/books/NBK537320/ , 6 Dietrich TJ, Sutter R, Froehlich JM, Pfirrmann CWA. Particulate versus non-particulate steroids for lumbar transforaminal or interlaminar epidural steroid injections: an update. Skeletal Radiology. 2014;44(2):149-155. doi:10.1007/s00256-014-2048-6
Non-particulate steroids
Water-soluble or non-particulate steroids have smaller particle sizes and do not aggregate together. They typically stay in the epidural space for a shorter duration of time and are thought to have short-term pain-relieving effects. Dexamethasone is an example of non-particulate steroids. 4 Chang, Douglas, Zlomislic, Vinko. Chapter 273. Lumbar Spinal Injections. In: Chapman, Michael W. Chapman's Orthopaedic Surgery. Philadelphia: Lippincott Williams & Wilkins. https://www.researchgate.net/publication/327034223_Lumbar_spinal_injections_Chapman's_Orthopaedic_Surgery_Chapter_273. Accessed June 26, 2019. , 5 Hassan KZ, Sherman Al. Epidural Steroids. [Updated 2019 May 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-.Available from: https://www.ncbi.nlm.nih.gov/books/NBK537320/ , 6 Dietrich TJ, Sutter R, Froehlich JM, Pfirrmann CWA. Particulate versus non-particulate steroids for lumbar transforaminal or interlaminar epidural steroid injections: an update. Skeletal Radiology. 2014;44(2):149-155. doi:10.1007/s00256-014-2048-6
Combining Steroids and Local Anesthetics May Provide Enhanced Pain Relief
While some injection preparations use pure steroids, others mix local anesthetics in the steroid solution for enhanced pain relief. Local anesthetics act relatively faster than steroids and help reduce pain signals from inflamed nerves. 4 Chang, Douglas, Zlomislic, Vinko. Chapter 273. Lumbar Spinal Injections. In: Chapman, Michael W. Chapman's Orthopaedic Surgery. Philadelphia: Lippincott Williams & Wilkins. https://www.researchgate.net/publication/327034223_Lumbar_spinal_injections_Chapman's_Orthopaedic_Surgery_Chapter_273. Accessed June 26, 2019. Lidocaine and bupivacaine are commonly used local anesthetics in epidural steroid injections. 3 Patel K, Upadhyayula S. Epidural Steroid Injections. [Updated 2019 May 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470189/
Exploring the Techniques of Epidural Steroid Injections
An epidural injection can be administered using various techniques.
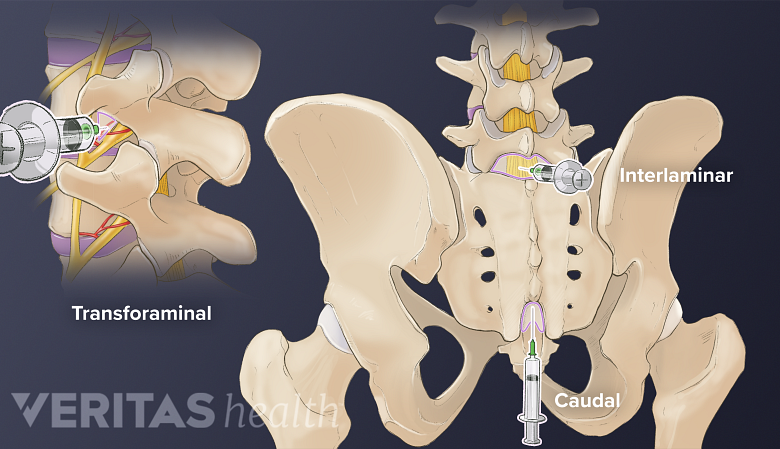
Typically, 1 of 3 techniques are used in an epidural steroid injection: transforaminal, interlaminar, and caudal. Each method fills the epidural space differently and deposits the medication in a different location within the space. The effectiveness of a technique depends on its ability to deliver the medication closer to the target nerve roots.
Transforaminal injection
This method is considered the most effective in depositing the solution close to the affected nerve roots. It may be used if sciatica is caused by certain lower back conditions, such as a lumbar herniated disc impinging a spinal nerve.
In this method, the needle is inserted through the side of the spinal canal into the intervertebral foramen to reach the epidural space. To avoid adjacent blood vessel damage, the needle is passed through a small space above the spinal nerve as it exits the neuroforamen, called the safe triangle. 2 Manchikanti L, Kaye AD, Falco FJE, Hirsch JA. Essentials of Interventional Techniques in Managing Chronic Pain. Cham, Switzerland: Springer; 2018.
Interlaminar injection
In this method, the needle is inserted through the back of the spinal canal between adjacent spinous processes (bony projection of the vertebra) or laminae (posterior wall of the vertebra) to reach the epidural space. 2 Manchikanti L, Kaye AD, Falco FJE, Hirsch JA. Essentials of Interventional Techniques in Managing Chronic Pain. Cham, Switzerland: Springer; 2018.
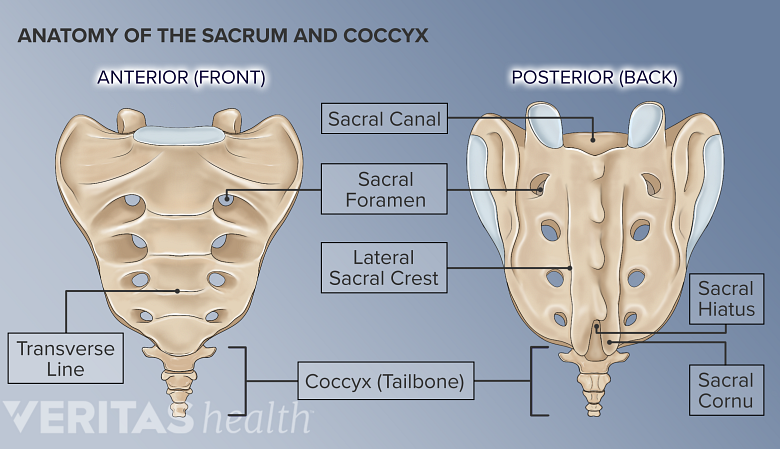
Caudal injection
The sacral hiatus contains several nerves that leave the sacral canal.
In this technique, the needle is inserted from below the spinal canal through an opening called the sacral hiatus. The depth of penetration of the needle to reach the epidural space is more in this method. While this method is safer and easier to perform, it is also less effective. 2 Manchikanti L, Kaye AD, Falco FJE, Hirsch JA. Essentials of Interventional Techniques in Managing Chronic Pain. Cham, Switzerland: Springer; 2018.
In general, the location and severity of the spinal inflammation, injection technique used, and the proximity of the medication to the affected nerve roots—all contribute to the final outcome of the injection. It is also important that the injection is delivered under the guidance of contrast-enhanced fluoroscopy (live -x-ray) for safety and accuracy.
- 1 Manchikanti L, Kaye AD, Manchikanti K, Boswell M, Pampati V, Hirsch J. Efficacy of Epidural Injections in the Treatment of Lumbar Central Spinal Stenosis; A Systematic Review. Anesthesiology and Pain Medicine. 2015;5(1). doi:10.5812/aapm.23139
- 2 Manchikanti L, Kaye AD, Falco FJE, Hirsch JA. Essentials of Interventional Techniques in Managing Chronic Pain. Cham, Switzerland: Springer; 2018.
- 3 Patel K, Upadhyayula S. Epidural Steroid Injections. [Updated 2019 May 2]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470189/
- 4 Chang, Douglas, Zlomislic, Vinko. Chapter 273. Lumbar Spinal Injections. In: Chapman, Michael W. Chapman's Orthopaedic Surgery. Philadelphia: Lippincott Williams & Wilkins. https://www.researchgate.net/publication/327034223_Lumbar_spinal_injections_Chapman's_Orthopaedic_Surgery_Chapter_273. Accessed June 26, 2019.
- 5 Hassan KZ, Sherman Al. Epidural Steroids. [Updated 2019 May 10]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2019 Jan-.Available from: https://www.ncbi.nlm.nih.gov/books/NBK537320/
- 6 Dietrich TJ, Sutter R, Froehlich JM, Pfirrmann CWA. Particulate versus non-particulate steroids for lumbar transforaminal or interlaminar epidural steroid injections: an update. Skeletal Radiology. 2014;44(2):149-155. doi:10.1007/s00256-014-2048-6