Neck pain can take on various forms, ranging anywhere from a dull and irritating ache to burning, debilitating nerve pain that may radiate down the shoulder and into the arm. There can also be wide variations in how the pain started and how long it may last. In order to develop an effective treatment plan, it is essential to understand different neck pain types.
This article explains 4 types of neck pain and highlights differences between short-term acute pain and long-lasting chronic pain.
In This Article:
- Types of Neck Pain
- Understanding Acute vs. Chronic Neck Pain
Axial Neck Pain
Axial pain is confined to a specific area of the neck and does not radiate elsewhere.
The most common type of neck pain is axial pain, also called mechanical pain. Axial pain is focused on one part or region of the neck and does not move or radiate. It typically feels dull, achy, or throbbing but can also be sharp or stinging. Symptoms may increase with certain movements or poor posture.
Neck muscle strains and/or ligament sprains are typical causes of axial neck pain. Other sources of axial neck pain include various mechanisms related to spinal degeneration or trauma, including cervical disc degeneration, facet joint dysfunction, or vertebral bone fracture.
Radicular Pain
Radicular pain radiates into the arms and shoulder along the path of the spinal nerve root.
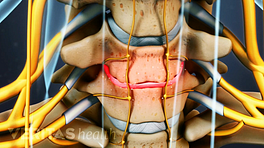
Radicular pain can occur when a nerve root in the cervical spine becomes inflamed, causing pain to radiate along the nerve, down into the shoulder, arm, and/or hand.
Radicular pain involves the nerve, and nerve pain can feel searing or electric shock-like. The pain can intensify with certain movements and posture. It is typically experienced on only one side of the body, but it can be on both.
When radicular pain stems from the cervical spine, it is usually due to spinal degeneration, such as when a nerve root is irritated by bony overgrowths, called Osteophytes (bone spurs), or a cervical herniated disc.
The location of radicular pain is commonly thought to follow dermatomal patterns (areas of the skin served by a single nerve cell). Some studies, however, have indicated that radicular pain does not always follow this pattern. 1 Murphy DR, Hurwitz EL, Gerrard JK, Clary R. Pain patterns and descriptions in patients with radicular pain: Does the pain necessarily follow a specific dermatome? Chiropr Osteopat. 2009; 17: 9.
Referred Pain
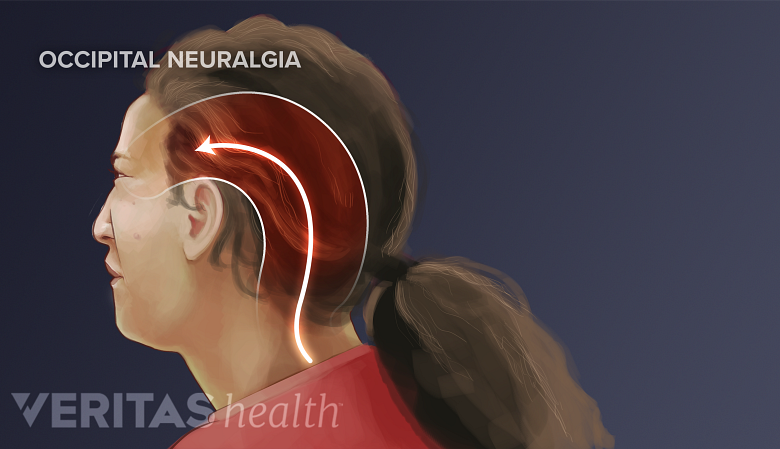
Neck problems may lead to referred pain, often causing headaches.
When pain is experienced in a location other than its source and is not caused by nerve root irritation, it is called referred pain. It is usually experienced as a deep, achy, cramping and/or throbbing sensation. The area of distribution is likely to be more diffuse, or spread out, than radiating pain, but these two types of pain can feel similar. Referred pain is typically felt on only one side of the body, but it can be on both.
The mechanisms of how referred pain develops and spreads are still being studied. For example, when a trigger point (tender or hypersensitive part of a muscle) is compressed, the pain symptoms can be referred to other parts of the body. However, there is no firm agreement in the medical community about how trigger points develop and whether their pain patterns are predictable. 2 Bron C, Dommerholt JD. Etiology of myofascial trigger points. Curr Pain Headache Rep. 2012. 16(5): 439–444. doi: 10.1007/s11916-012-0289-4.
Pain can be referred to the neck in various ways, such as from the heart (during a heart attack) or jaw (temporomandibular joint). Conversely, a pathology in the neck can cause referred pain in other parts of the body, most commonly a headache, shoulder pain, or upper back pain.
Myelopathic Pain
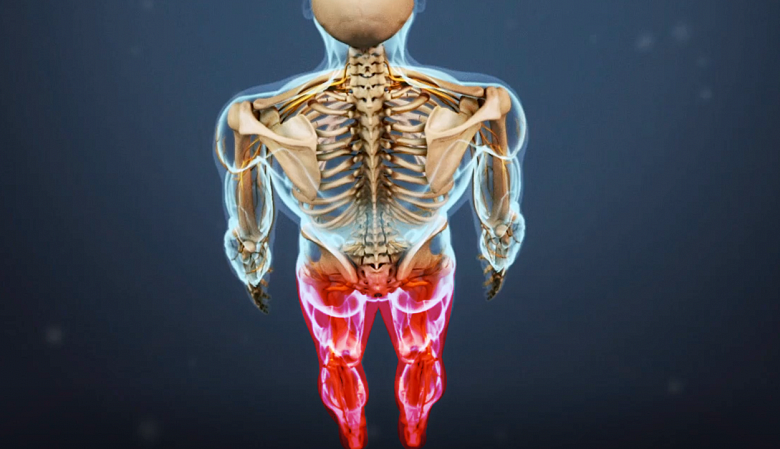
Rarely, myelopathy in the neck may cause pain in the legs and feet.
When the spinal cord in the neck becomes compressed, myelopathic pain may develop. While myelopathic pain may occur at the level of compression causing neck pain, symptoms are often located at a distance below the neck/compression site, such as in the legs and/or feet. This separation of symptoms and causal region may contribute to an increased risk for misdiagnosis and mismanagement. 3 Chan CK, Lee H-Y, Choi W-C, Cho JY, Lee S-H. Cervical cord compression presenting with sciatica-like leg pain. Eur Spine J. 2011 Jul; 20(Suppl 2): 217-221. doi: 10.1007/s00586-010-1585-5.
See Cervical Stenosis with Myelopathy and Cervical Spondylosis with Myelopathy
Funicular pain is another type of spinal cord-related pain and may occur when the cord’s ascending tracts—the spinothalmic or posterior column tracts—become compressed or irritated. Funicular pain tends to present as an achy, throbbing, or cold feeling in one of the limbs, such as a leg, or in the trunk of the body. It can also feel electric shock-like and similar to radicular pain (sciatica) going down the leg. Sometimes funicular pain is experienced when the neck is flexed forward, known as Lhermitte’s phenomenon, and results in a searing pain that can travel down the spine and/or into the arms or legs. 4 Darby SA. Neurologic evaluation of the cervical spine. In: Benzel EC, The Cervical Spine, 5th Edition. Philadelphia, PA: Lippinscott Williams & Wilkins; 2012: 167.
Several Pain Types Can Exist Together
Any of these pain types can occur alone or in combination with one or more others. For example, it can be difficult to distinguish between radicular pain and referred pain, and some spinal pathologies can lead to both types of pain.
- 1 Murphy DR, Hurwitz EL, Gerrard JK, Clary R. Pain patterns and descriptions in patients with radicular pain: Does the pain necessarily follow a specific dermatome? Chiropr Osteopat. 2009; 17: 9.
- 2 Bron C, Dommerholt JD. Etiology of myofascial trigger points. Curr Pain Headache Rep. 2012. 16(5): 439–444. doi: 10.1007/s11916-012-0289-4.
- 3 Chan CK, Lee H-Y, Choi W-C, Cho JY, Lee S-H. Cervical cord compression presenting with sciatica-like leg pain. Eur Spine J. 2011 Jul; 20(Suppl 2): 217-221. doi: 10.1007/s00586-010-1585-5.
- 4 Darby SA. Neurologic evaluation of the cervical spine. In: Benzel EC, The Cervical Spine, 5th Edition. Philadelphia, PA: Lippinscott Williams & Wilkins; 2012: 167.