Treatment for vertebral osteomyelitis is usually conservative (meaning nonsurgical) and based primarily on use of intravenous antibiotic treatment. Occasionally, surgery may be necessary to alleviate pressure on the spinal nerves, clean out infected material, and/or stabilize the spine.
In This Article:
- Osteomyelitis, a Spinal Infection
- Osteomyelitis Symptoms
- Osteomyelitis Diagnosis
- Osteomyelitis Treatments
Nonsurgical Treatments for Vertebral Osteomyelitis
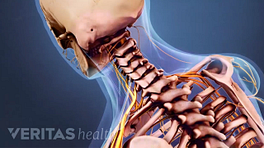
Bracing may help to enhance spinal stability during healing.
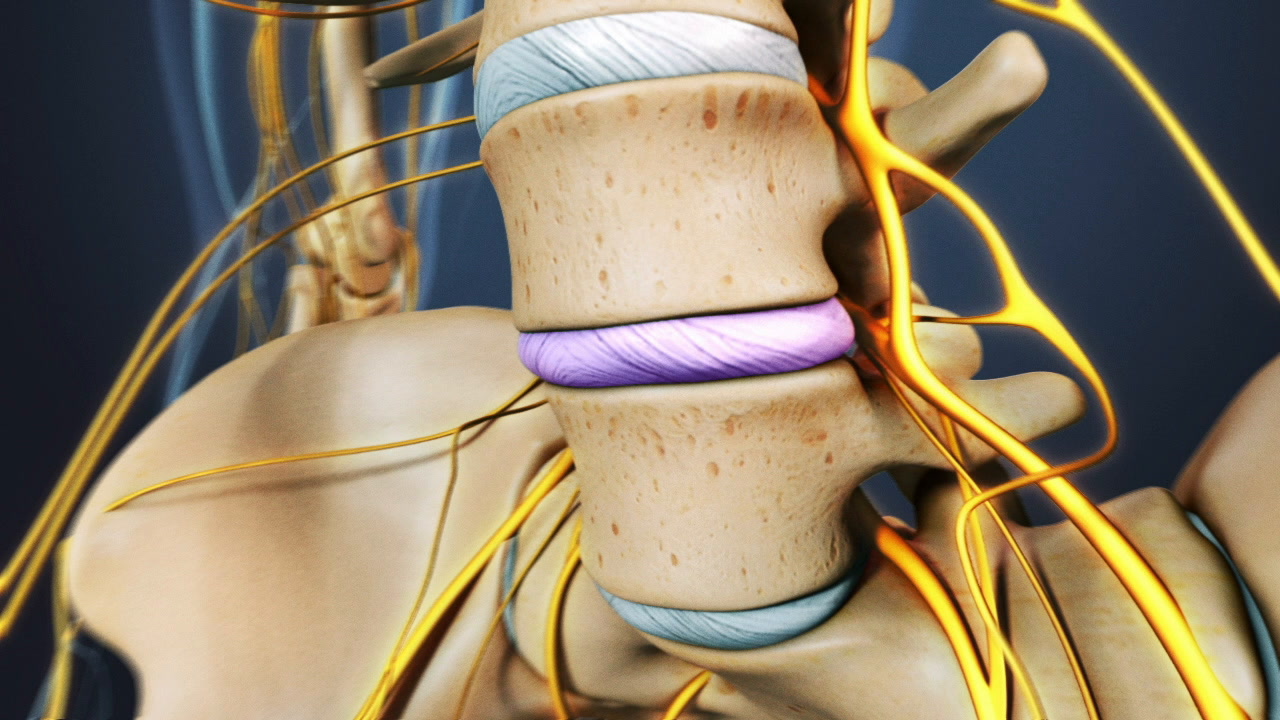
Treatment for a spinal infection usually includes a combination of intravenous antibiotic therapy, bracing, and rest.
Most cases of vertebral osteomyelitis are caused by Staphylococcus Aureus, which is generally very sensitive to antibiotics. The intravenous antibiotic treatment usually takes about four weeks, and then is usually followed by about two weeks of oral antibiotics. For infection caused by tuberculosis, patients are often required to take three drugs for up to one year.
Bracing is recommended to provide stability for the spine while the infection is healing. It is usually continued for 6 to 12 weeks, until either a bony fusion is seen on X-ray, or until the patient’s pain subsides. A rigid brace works best and need only be worn when the patient is active.
Surgical Treatments and Considerations
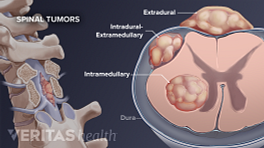
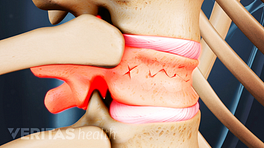
Surgical decompression is necessary if an epidural abscess places pressure on the neural elements. Because surgical decompression often destabilizes the spine further, instrumentation and fusion are also frequently included to prevent worsening deformity and pain.
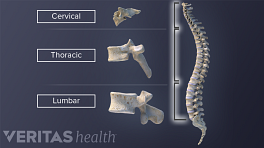
If the infection does not respond to antibiotic therapy, surgical debridement and removal of infected material may be necessary. Most infections are predominantly in the anterior structures (such as the vertebral body) and the debridement is best done through an anterior (front) approach. Stabilization and fusion are also done after removing the infected bone.
See Anterior and Posterior Lumbar Fusion Surgery
Surgery may also be necessary if there is a great deal of bony destruction with resultant deformity and pain. Reconstructing the bony elements and stabilizing the spine can help reduce pain and prevent further collapse of the spine. The surgery usually needs to be done from a combined anterior (front) and posterior (back) approach.
Bone graft from the patient’s hip is usually used in the front of the spine, where most of the infection is located, rather than metal implants. It is controversial whether or not the use of metal implants decreases the risk of eradicating the infection.
Bone grafting for anterior column support (in the front of the spine) is usually followed by posterior instrumentation (in the back of the spine), which places the hardware in a relatively clean environment and decreases the chance of a bacterial infection around the hardware.