Magnetic resonance imaging (MRI) is a highly sensitive and specific imaging technique that yields comprehensive images of the structure, function, and composition of tissues in the body. 1 Balasubramanya R, Selvarajan SK. Lumbar Spine Imaging. [Updated 2022 Mar 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK553181/ , 2 Chan RW, Lau JYC, Lam WW, Lau AZ. Magnetic resonance imaging. In: Encyclopedia of Biomedical Engineering. Elsevier; 2019:574-587. doi: https://doi.org/10.1016/B978-0-12-801238-3.99945-8 The technique uses a strong magnet, radio waves, and a computer to generate detailed images of the body. In the spine, an MRI scan can reveal thorough details of the joints, muscles, tendons, ligaments, spinal discs, spinal nerve roots, and the spinal cord.
Watch Video: Should You Get an MRI on Your First Visit?
MRI produces detailed images without the use of ionizing radiation, making it a safer option compared to standard imaging techniques, like x-rays or computed tomography (CT) scans.
In This Article:
When a Spinal MRI Scan Is Recommended
MRI scans help diagnose herniated discs, spinal cord compression, spinal tumors, and more.
For neck or back pain, MRI is typically recommended when relief of symptoms is not obtained after a series of first-line treatments have been tried for several weeks. It serves as a diagnostic tool to further investigate the anatomical source of pain and to determine the exact cause or locate the precise site of injury.
MRI may be recommended on an urgent basis when the following conditions are suspected:
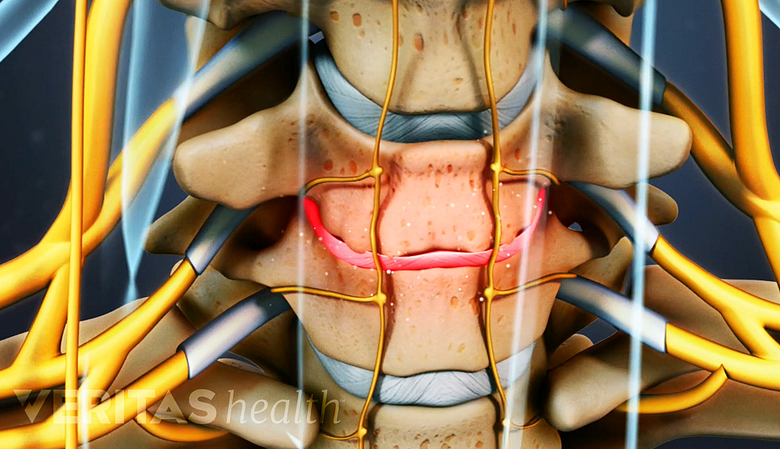
- Spinal cord compression in the neck due to conditions such as cervical stenosis with myelopathy 3 Tempest-Mitchell J, Hilton B, Davies BM, et al. A comparison of radiological descriptions of spinal cord compression with quantitative measures, and their role in non-specialist clinical management. Sherman JH, ed. PLoS ONE. 2019;14(7):e0219380. doi:https://doi.org/10.1371/journal.pone.0219380
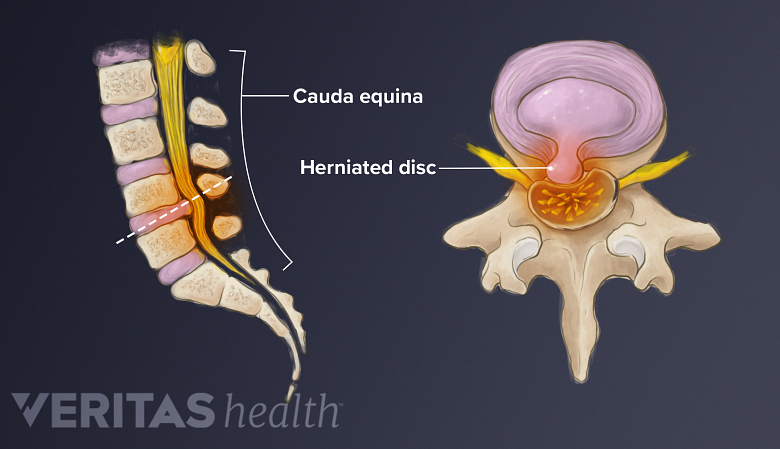
- Spinal cord compression in the lower back, leading to conditions such as cauda equina syndrome 4 Fairbank J, Hashimoto R, Dailey A, Patel AA, Dettori JR. Does patient history and physical examination predict MRI proven cauda equina syndrome?. Evid Based Spine Care J. 2011;2(4):27-33. doi:10.1055/s-0031-1274754
- Primary or secondary spinal tumors 5 Ziu E, Viswanathan VK, Mesfin FB. Spinal Metastasis. [Updated 2022 Mar 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441950/
- Herniated disc that causes radiculopathy 6 Amin RM, Andrade NS, Neuman BJ. Lumbar Disc Herniation. Curr Rev Musculoskelet Med. 2017;10(4):507-516. doi:10.1007/s12178-017-9441-4
In these conditions, MRI is considered the gold standard for imaging and investigating the underlying cause of the specific condition and formulating the treatment plan. 3 Tempest-Mitchell J, Hilton B, Davies BM, et al. A comparison of radiological descriptions of spinal cord compression with quantitative measures, and their role in non-specialist clinical management. Sherman JH, ed. PLoS ONE. 2019;14(7):e0219380. doi:https://doi.org/10.1371/journal.pone.0219380 , 4 Fairbank J, Hashimoto R, Dailey A, Patel AA, Dettori JR. Does patient history and physical examination predict MRI proven cauda equina syndrome?. Evid Based Spine Care J. 2011;2(4):27-33. doi:10.1055/s-0031-1274754 , 5 Ziu E, Viswanathan VK, Mesfin FB. Spinal Metastasis. [Updated 2022 Mar 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441950/ , 6 Amin RM, Andrade NS, Neuman BJ. Lumbar Disc Herniation. Curr Rev Musculoskelet Med. 2017;10(4):507-516. doi:10.1007/s12178-017-9441-4
Presurgical planning
MRI scans are typically used in planning any type of neck or back surgery (unless certain conditions preclude their use), such as a discectomy, artificial disc replacement, spinal fusion, or metastatic spinal tumor surgery.
- The level of detail an MRI provides can help determine the extent of spinal injury and the approach to surgery.
- When a previous back surgery has been performed, MRI scans with and without contrast can help differentiate scar tissue from a hematoma or recurrent disc herniation.
- Prior to administering an epidural steroid injection, if a tumor or infection is suspected, an MRI scan can help determine if the injection is safe and appropriate, and if so, prevent injecting into the tumor or infection.
In certain circumstances, MRI scans may help assess postsurgical healing and recovery.
What an MRI Scan Can Reveal about Back or Neck Pain
An MRI scan can reveal spinal tissue changes, such as degeneration.
Diagnostic information gleaned from an MRI scan may reveal changes in the anatomy and structure of spinal tissues, such as:
- Degeneration
- Disc desiccation (dehydration)
- Inflammation
- Swelling
- Compression
- Abnormal growth(s)
On spinal MRI scans, these changes are useful in identifying pathologies related to the spinal discs, cartilaginous endplates on the top and bottom of each spinal bone (vertebra), and nervous tissue, including spinal nerves and the spinal cord.
The findings from the patient’s physical exam and medical history are correlated with the information gathered from an MRI scan to arrive at a working clinical diagnosis.
MRI with Contrast
For certain conditions, an additional MRI sequence using contrast can help more accurately determine the anatomy and pathology of the area of the spine being studied. These contrast agents make the abnormality in the tissues brighter and clearer—helping doctors identify the pathology with greater precision.
- MRI with contrast is typically used to help detect abnormalities in the blood vessels. 7 Meng, Xiao-xi; Zhang, Yong-qiu; Liao, Hua-qiang; Liu, Hong-chao; Jiang, Hai-lin; Ke, Shu-jun; Dong, Wei-hua (2016). Dynamic contrast-enhanced MRI for the assessment of spinal tumor vascularity: correlation with angiography. European Spine Journal, 25(12), 3952–3961. doi:10.1007/s00586-016-4713-z The contrast agent tends to accumulate and outline tissues with abnormal vessels, such as scar tissue, infection, and spinal tumors.
- In the spine, MRI with contrast is widely used to study spinal tumors. The size and properties of the tumor are revealed through these contrast scans and help physicians treating spinal tumors plan the next treatment steps. 7 Meng, Xiao-xi; Zhang, Yong-qiu; Liao, Hua-qiang; Liu, Hong-chao; Jiang, Hai-lin; Ke, Shu-jun; Dong, Wei-hua (2016). Dynamic contrast-enhanced MRI for the assessment of spinal tumor vascularity: correlation with angiography. European Spine Journal, 25(12), 3952–3961. doi:10.1007/s00586-016-4713-z
The most commonly used, FDA-approved agents are gadolinium-based contrast agents (GBCA). 7 Meng, Xiao-xi; Zhang, Yong-qiu; Liao, Hua-qiang; Liu, Hong-chao; Jiang, Hai-lin; Ke, Shu-jun; Dong, Wei-hua (2016). Dynamic contrast-enhanced MRI for the assessment of spinal tumor vascularity: correlation with angiography. European Spine Journal, 25(12), 3952–3961. doi:10.1007/s00586-016-4713-z Gadolinium is a rare earth metal. In its natural state, this metal is toxic to humans. Gadolinium undergoes a series of purification processes to make it safe for use in humans. The GBCA solution is injected into a vein in the patient’s arm, and its silvery-white color reacts with the abnormal cells in the body making them clearer on an MRI scan. After a few hours, gadolinium is expelled from the body in the urine.
In rare cases, gadolinium may cause serious cardiovascular, kidney, or respiratory complications. 8 Ibrahim MA, Hazhirkarzar B, Dublin AB. Gadolinium Magnetic Resonance Imaging. [Updated 2022 Jul 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482487/
To minimize the risk of kidney complications, blood work may be ordered prior to the MRI with contrast in some individuals who have chronic or severe kidney disease or are at potential risk from the contrast. The blood work may help analyze if the kidneys can metabolize and filter gadolinium if it is injected into the body. 9 Weinreb JC, Rodby RA, Yee J, et al. Use of intravenous gadolinium-based contrast media in patients with kidney disease: consensus statements from the american college of radiology and the national kidney foundation. Radiology. 2021;298(1):28-35. doi:10.1148/radiol.2020202903 , 10 Mathur M, Jones JR, Weinreb JC. Gadolinium deposition and nephrogenic systemic fibrosis: a radiologist’s primer. RadioGraphics. 2020;40(1):153-162. doi:10.1148/rg.2020190110
How an MRI Machine Creates an Image
An MRI scanner images the spine by using strong magnets that align the hydrogen atoms inside the body’s cells in the area to be studied to match the magnet’s magnetic field.
- Radiofrequency waves are sent to the same body part to intentionally disrupt the alignment of hydrogen atoms.
- The radiofrequency pulse is then turned off so that the hydrogen atoms realign again.
- The atomic changes from these magnetic and radiofrequency waves are detected by a receiver in the MRI scanner, which constructs the MRI images using special software in the scanner.
- The scanned images are viewed on a computer screen that is connected to the MRI scanner.
MRI scans are read and interpreted by a radiologist.
Types of MRI Machines
The design of a standard MRI machine is closed-bore, which means that the patient lies in a narrow cylindrical tunnel that houses the machine’s magnet.
For patients with specific needs, such as those with larger body habitus, who feel claustrophobic, or have specific spinal conditions, the following machine types may be beneficial:
- Wide-bore MRI machine, which uses a wider tunnel compared to the standard closed-bore machine, but still closes around the body.
- Open MRI machine, which allows for more space and comfort during the scan and does not enclose the patient. An open MRI may be used if a standard MRI is too small or uncomfortable.
- Upright MRI machine, which allows the spine to be scanned while sitting up (called an upright MRI scan). An upright MRI scan accurately represents the pressure on the spine in a seated posture and the health of the spinal tissues in this position.
- Weight-bearing MRI machine, which simulates the weight placed on the spine in a standing posture. This modification allows the image produced to show how weight bearing affects the spine.
The type of MRI used depends on the suspected cause of pain or the patient’s need. For example, spinal stenosis symptoms tend to feel worse when standing, and an upright or weight-bearing MRI scan may be more appropriate. A patient with obesity or someone who feels claustrophobic may benefit from using a wide-bore or open MRI machine.
Preparing for an MRI Scan
Prior to an MRI scan, the patient is typically asked to change into a hospital gown and remove all jewelry and accessories, as metals will be affected by the magnet. Additionally, the technician enquires about any dental fillings and metallic implants that may complicate the scan and/or damage the implant.
The scan can take 15 minutes to an hour depending on the area being scanned and the number of scan sequences needed.
Step-By-Step Guide to an MRI Scan
An MRI scan is conducted in a scanner room that provides protective shielding from the strong magnetic field created by the magnet in the MRI scanner. The scanner room houses the MRI machine and has an adjacent control area, where the MRI technician controls the machine.
An MRI scan usually follows a standard protocol.
- The patient lies face up on a small table with their arms at their sides. The table glides into a cylindrical magnetic resonance (MR) scanner machine, which is open at both ends.
- If a contrast MRI is needed, the contrast agent is injected through an intravenous (IV) route into a vein in the arm prior to the scan.
- During the procedure, instructions may be provided through a small speaker. When scanners are in operation, loud clicking noises are produced. The technician may provide earplugs or noise-canceling headphones to protect the patient’s hearing.
- The technician initiates the scanning process.
- Patients are required to stay very still and breathe normally while the scans are being produced, as any movement may cause artifacts or reduce the quality of the scanned image.
- The procedure causes no pain, and nothing can be felt when the body is exposed to the strong magnetic field within the scanner.
- After a series of scans are taken, the patient is notified, and they can relax for a few seconds until the next set of scans are captured.
- Once all the scans are taken from different angles, the machine is turned off and the patient can get dressed.
During an MRI procedure, the technologist will be able to talk to and hear the patient at all times.
Anti-anxiety medication or mild sedation may be recommended if claustrophobia or anxiety during the scan is a concern. Patients who are injected with gadolinium-based contrast agents are advised to drink a few glasses of water after the procedure to help clear the contrast agent from their bodies.
Unless sedation is used, regular activity can be continued after the scan with no extra precautions.
Limitations of Spinal MRI
An MRI scan is highly sensitive and picks up the slightest anatomic variation in the body’s tissues. The scan cannot distinguish between natural, painless wear and tear and painful degeneration in the spinal column. MRI scans that show severe age-related degeneration may be found in patients with no pain, while some scans that reveal mild degeneration may belong to patients with significant pain. These scenarios demonstrate that the findings of an MRI scan do not always correlate with symptoms— and that a scan on its own cannot accurately diagnose the cause of pain. 11 Brinjikji W, Luetmer PH, Comstock B, et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol. 2014;36(4):811-6. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4464797/ , 12 Rao D, Scuderi G, Scuderi C, Grewal R, Sandhu SJ. The Use of Imaging in Management of Patients with Low Back Pain. J Clin Imaging Sci. 2018;8:30. Published 2018 Aug 24. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6118107/
For this reason, while diagnosing back pain, an MRI is interpreted within the context of a physical exam, medical history, and the symptoms experienced by the patient.
- 1 Balasubramanya R, Selvarajan SK. Lumbar Spine Imaging. [Updated 2022 Mar 9]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK553181/
- 2 Chan RW, Lau JYC, Lam WW, Lau AZ. Magnetic resonance imaging. In: Encyclopedia of Biomedical Engineering. Elsevier; 2019:574-587. doi: https://doi.org/10.1016/B978-0-12-801238-3.99945-8
- 3 Tempest-Mitchell J, Hilton B, Davies BM, et al. A comparison of radiological descriptions of spinal cord compression with quantitative measures, and their role in non-specialist clinical management. Sherman JH, ed. PLoS ONE. 2019;14(7):e0219380. doi:https://doi.org/10.1371/journal.pone.0219380
- 4 Fairbank J, Hashimoto R, Dailey A, Patel AA, Dettori JR. Does patient history and physical examination predict MRI proven cauda equina syndrome?. Evid Based Spine Care J. 2011;2(4):27-33. doi:10.1055/s-0031-1274754
- 5 Ziu E, Viswanathan VK, Mesfin FB. Spinal Metastasis. [Updated 2022 Mar 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441950/
- 6 Amin RM, Andrade NS, Neuman BJ. Lumbar Disc Herniation. Curr Rev Musculoskelet Med. 2017;10(4):507-516. doi:10.1007/s12178-017-9441-4
- 7 Meng, Xiao-xi; Zhang, Yong-qiu; Liao, Hua-qiang; Liu, Hong-chao; Jiang, Hai-lin; Ke, Shu-jun; Dong, Wei-hua (2016). Dynamic contrast-enhanced MRI for the assessment of spinal tumor vascularity: correlation with angiography. European Spine Journal, 25(12), 3952–3961. doi:10.1007/s00586-016-4713-z
- 8 Ibrahim MA, Hazhirkarzar B, Dublin AB. Gadolinium Magnetic Resonance Imaging. [Updated 2022 Jul 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482487/
- 9 Weinreb JC, Rodby RA, Yee J, et al. Use of intravenous gadolinium-based contrast media in patients with kidney disease: consensus statements from the american college of radiology and the national kidney foundation. Radiology. 2021;298(1):28-35. doi:10.1148/radiol.2020202903
- 10 Mathur M, Jones JR, Weinreb JC. Gadolinium deposition and nephrogenic systemic fibrosis: a radiologist’s primer. RadioGraphics. 2020;40(1):153-162. doi:10.1148/rg.2020190110
- 11 Brinjikji W, Luetmer PH, Comstock B, et al. Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol. 2014;36(4):811-6. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4464797/
- 12 Rao D, Scuderi G, Scuderi C, Grewal R, Sandhu SJ. The Use of Imaging in Management of Patients with Low Back Pain. J Clin Imaging Sci. 2018;8:30. Published 2018 Aug 24. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6118107/