Spondylolisthesis is Latin for "slipped vertebral body," and is diagnosed when one vertebra slips forward over the one below.
Degenerative spondylolisthesis may occur as part of the normal aging process of the spine. It may alter normal spinal alignment. 1 Akkawi I, Zmerly H. Degenerative Spondylolisthesis: A Narrative Review. Acta Biomed. 2022 Jan 19;92(6):e2021313. doi: 10.23750/abm.v92i6.10526. PMID: 35075090; PMCID: PMC8823594. , 2 Cushnie D, Johnstone R, Urquhart JC, Gurr KR, Bailey SI, Bailey CS. Quality of Life and Slip Progression in Degenerative Spondylolisthesis Treated Nonoperatively. Spine (Phila Pa 1976). 2018;43(10):E574-E579. doi:10.1097/BRS.0000000000002429
Degenerative spondylolisthesis typically occurs in the lumbar spine (low back). In most cases, the L4-L5 spinal segment is affected, followed by the L3-L4 and L5-S1 spinal segments. 1 Akkawi I, Zmerly H. Degenerative Spondylolisthesis: A Narrative Review. Acta Biomed. 2022 Jan 19;92(6):e2021313. doi: 10.23750/abm.v92i6.10526. PMID: 35075090; PMCID: PMC8823594.
In This Article:
4 Most Common Causes of Degenerative Spondylolisthesis
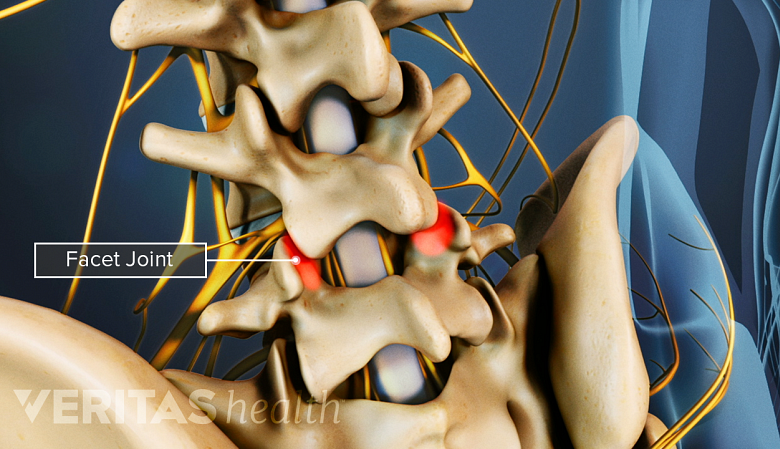
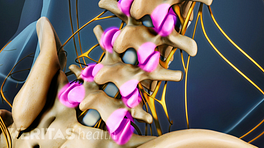
Age-related changes, like facet joint arthritis, may lead to degenerative spondylolisthesis.
Degenerative spondylolisthesis is attributed to age-related changes that can disrupt spinal alignment.
The specific changes include 1 Akkawi I, Zmerly H. Degenerative Spondylolisthesis: A Narrative Review. Acta Biomed. 2022 Jan 19;92(6):e2021313. doi: 10.23750/abm.v92i6.10526. PMID: 35075090; PMCID: PMC8823594. , 3 García-Ramos CL, Valenzuela-González J, Baeza-Álvarez VB, Rosales-Olivarez LM, Alpizar-Aguirre A, Reyes-Sánchez A. Degenerative spondylolisthesis I: general principles. Acta Ortop Mex. 2020;34(5):324-328. doi:10.35366/97997 :
- Degeneration of the spinal discs
- Loss of resilience and strength in the ligaments responsible for spinal stability
- Osteoarthritis of the facet joints that connect the vertebrae, resulting in less support for the spinal segment
- Inadequate muscle stabilization
Less commonly, pregnancy and participating in sports may accelerate degenerative changes in the spine, leading to spondylolisthesis. 4 Wang YXJ, Káplár Z, Deng M, Leung JCS. Lumbar degenerative spondylolisthesis epidemiology: A systematic review with a focus on gender-specific and age-specific prevalence. J Orthop Translat. 2016;11:39-52. Published 2016 Dec 1. doi:10.1016/j.jot.2016.11.001
How Degenerative Spondylolisthesis Develops: The Role of the 3-Joint Complex
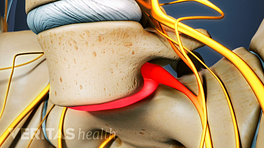
Spondylolisthesis occurs as a result of spinal motion segment degeneration.
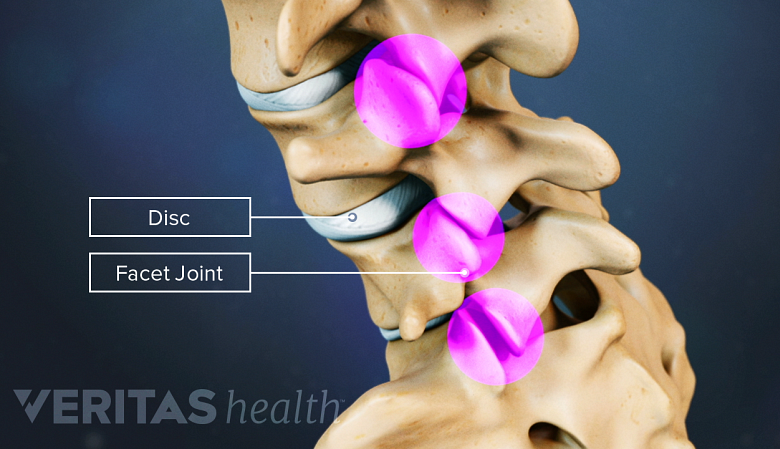
Spondylolisthesis develops due to degeneration at a spinal motion segment, which comprises a 3-joint complex. 5 Bernard F, Mazerand E, Gallet C, Troude L, Fuentes S. History of degenerative spondylolisthesis: From anatomical description to surgical management. Neurochirurgie. 2019;65(2-3):75-82. doi:10.1016/j.neuchi.2019.03.006 This 3-joint complex includes:
- A disc in the front, which acts as a shock absorber between adjacent vertebrae (bones that make up the spinal column)
- A pair of facet joints in the back, which allow limited motion. The facet joints may bear weight and limit spinal forward bending (flexion), backward bending (extension), rotation, and side-to-side motion.
Aging-related degeneration of the facets and discs may make them less able to bear loads, resulting in vertebral slippage in load-bearing segments of the lower spine. 3 García-Ramos CL, Valenzuela-González J, Baeza-Álvarez VB, Rosales-Olivarez LM, Alpizar-Aguirre A, Reyes-Sánchez A. Degenerative spondylolisthesis I: general principles. Acta Ortop Mex. 2020;34(5):324-328. doi:10.35366/97997
2 Types of Vertebral Slippage in Degenerative Spondylolisthesis
Vertebral slippage can occur symmetrically when both facets are equally affected.
Vertebral slippage in degenerative spondylolisthesis can happen in two ways 3 García-Ramos CL, Valenzuela-González J, Baeza-Álvarez VB, Rosales-Olivarez LM, Alpizar-Aguirre A, Reyes-Sánchez A. Degenerative spondylolisthesis I: general principles. Acta Ortop Mex. 2020;34(5):324-328. doi:10.35366/97997 :
- Symmetrically, if both facets are equally affected and degenerated. In this case, the vertebra slips forward horizontally in a symmetrical manner.
- Asymmetrically, where one facet is more degenerated than the other, causing the slippage to occur asymmetrically, which usually results in rotation.
In either case, the spinal disc also slips forward along with the vertebra. 3 García-Ramos CL, Valenzuela-González J, Baeza-Álvarez VB, Rosales-Olivarez LM, Alpizar-Aguirre A, Reyes-Sánchez A. Degenerative spondylolisthesis I: general principles. Acta Ortop Mex. 2020;34(5):324-328. doi:10.35366/97997
Degenerative spondylolisthesis commonly occurs in the low back and is relatively rare in other parts of the spine. The condition may occur in the neck (cervical spondylolisthesis) due to degenerative changes in the cervical facet joints.
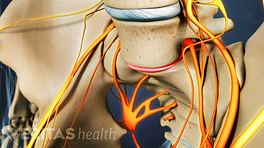
How Degenerative Spondylolisthesis Causes Pain
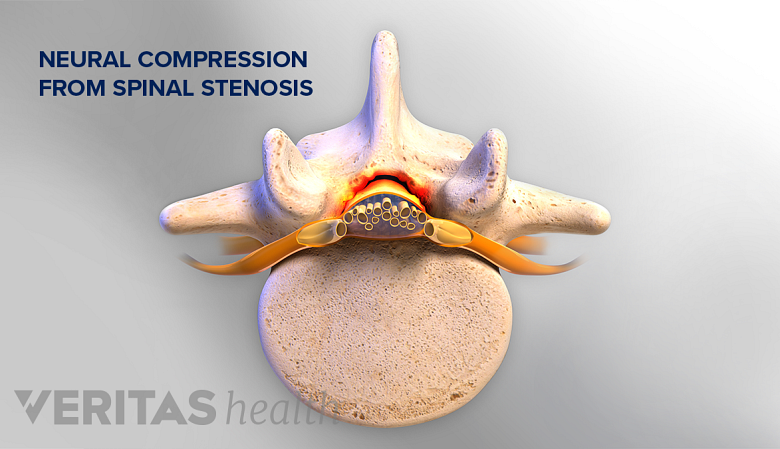
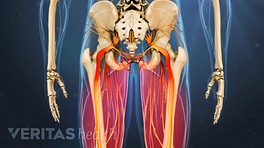
In degenerative spondylolisthesis, pain occurs due to neural compression from spinal stenosis.
Degenerative spondylolisthesis causes pain through one or more of the following processes 3 García-Ramos CL, Valenzuela-González J, Baeza-Álvarez VB, Rosales-Olivarez LM, Alpizar-Aguirre A, Reyes-Sánchez A. Degenerative spondylolisthesis I: general principles. Acta Ortop Mex. 2020;34(5):324-328. doi:10.35366/97997 :
- Joint pain: Degeneration of facet joints causes inflammation of the cartilaginous facet joint lining
- Soft tissue pain: Tension within the capsule and ligaments that surround the facet joints as the vertebra slips
- Muscle pain: Spasm of the muscles that support the affected spinal segment
- Stenosis pain: Narrowing of the central canal (spinal stenosis) and/or intervertebral foramen (foraminal stenosis) causing compression of the neural elements
These processes can result in some combination of localized back pain, sciatica, lumbar radiculopathy, and/or neurogenic claudication. 4 Wang YXJ, Káplár Z, Deng M, Leung JCS. Lumbar degenerative spondylolisthesis epidemiology: A systematic review with a focus on gender-specific and age-specific prevalence. J Orthop Translat. 2016;11:39-52. Published 2016 Dec 1. doi:10.1016/j.jot.2016.11.001
Hallmark Symptoms and Signs of Degenerative Spondylolisthesis
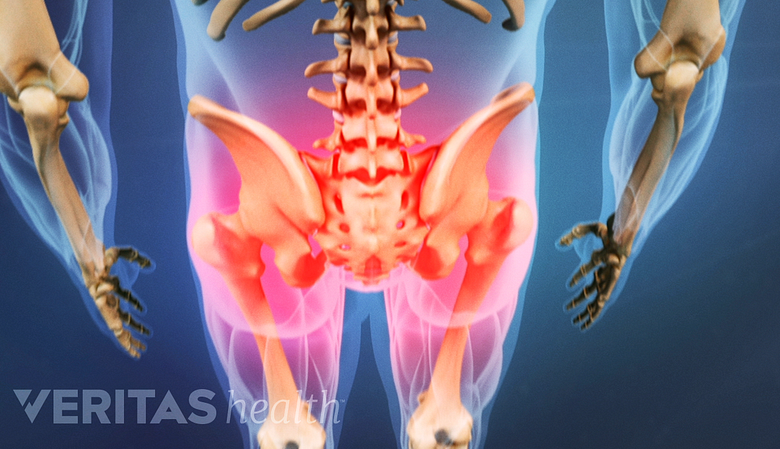
Back pain radiating to the buttocks is a common symptom of degenerative spondylolisthesis.
There’s a wide variation of spondylolisthesis symptoms. In general, the typical symptoms include some combination of 6 Matz PG, Meagher RJ, Lamer T, et al. North American Spine Society. Clinical Guidelines for Multidisciplinary Spine Care. Diagnosis and Treatment of Degenerative Lumbar Spondylolisthesis. 2nd ed; 2016. :
- Occasional back pain that comes and goes with increased activity
- Chronic low back pain
- Back pain with or without buttock, thigh, and/or leg pain (sciatica)
- Neurogenic claudication (leg pain while walking or standing for variable periods of time)
- Pain while bending backward (extension)
Less commonly, muscle spasm, tightness and a burning sensation, or sense of weakness may be felt in the lower back and/or thigh. 6 Matz PG, Meagher RJ, Lamer T, et al. North American Spine Society. Clinical Guidelines for Multidisciplinary Spine Care. Diagnosis and Treatment of Degenerative Lumbar Spondylolisthesis. 2nd ed; 2016.
The Grades of Degenerative Spondylolisthesis
A grading system, also called Meyerding’s classification, is used to measure the degree of slippage in spondylolisthesis. The grading relates to the amount the upper vertebral body slips forward on the lower vertebral body.
The amount of vertebral slip is measured via a side-view x-ray and then graded on a scale of 1 to 4. 7 Tenny S, Gillis CC. Spondylolisthesis. [Updated 2023 May 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430767/ In addition, flexion and extension x-rays (x-rays taken in the neutral, forward- and backward-bent positions) are performed to determine if there is any motion of one vertebra upon the other called translation or rotation.
| Grade of Degenerative Spondylolisthesis | Measurement of Vertebral Slippage |
|---|---|
| Grade 1 | <25% of the vertebral body has slipped forward |
| Grade 2 | 26% - 50% of the vertebral body has slipped forward |
| Grade 3 | 51% - 75% of the vertebral body has slipped forward |
| Grade 4 | 76% - 100% of the vertebral body has slipped forward |
In most cases, the degree of slippage is low and rarely exceeds grade 2. 1 Akkawi I, Zmerly H. Degenerative Spondylolisthesis: A Narrative Review. Acta Biomed. 2022 Jan 19;92(6):e2021313. doi: 10.23750/abm.v92i6.10526. PMID: 35075090; PMCID: PMC8823594. , 4 Wang YXJ, Káplár Z, Deng M, Leung JCS. Lumbar degenerative spondylolisthesis epidemiology: A systematic review with a focus on gender-specific and age-specific prevalence. J Orthop Translat. 2016;11:39-52. Published 2016 Dec 1. doi:10.1016/j.jot.2016.11.001
The Course of Degenerative Spondylolisthesis
The degree of degenerative spondylolisthesis may increase over time.
The body naturally employs several mechanisms to protect against further slippage, including:
- Formation of bone spurs (a normal response to changes in the amount of stress placed on bone)
- Hardening of bone (sclerosis)
- Deposition of calcium in the ligaments (ossification)
Because these mechanisms are relatively effective, the degree of degenerative spondylolisthesis is typically small. 4 Wang YXJ, Káplár Z, Deng M, Leung JCS. Lumbar degenerative spondylolisthesis epidemiology: A systematic review with a focus on gender-specific and age-specific prevalence. J Orthop Translat. 2016;11:39-52. Published 2016 Dec 1. doi:10.1016/j.jot.2016.11.001
For most people, degenerative spondylolisthesis is generally asymptomatic or causes mild symptoms that can be managed with nonsurgical treatments. 2 Cushnie D, Johnstone R, Urquhart JC, Gurr KR, Bailey SI, Bailey CS. Quality of Life and Slip Progression in Degenerative Spondylolisthesis Treated Nonoperatively. Spine (Phila Pa 1976). 2018;43(10):E574-E579. doi:10.1097/BRS.0000000000002429
How long degenerative spondylolisthesis takes to heal
The most common case is a low-grade spondylolisthesis without neurological symptoms (symptoms that radiate to the leg, or sciatica), and these typically get better within 1 year of using targeted nonsurgical treatment. 8 Samuel AM, Moore HG, Cunningham ME. Treatment for Degenerative Lumbar Spondylolisthesis: Current Concepts and New Evidence. Curr Rev Musculoskelet Med. 2017 Dec;10(4):521-529. doi: 10.1007/s12178-017-9442-3. PMID: 28994028; PMCID: PMC5685964.
Higher grades of vertebral slippage are rare and may sometimes need surgical treatment.
What makes degenerative spondylolisthesis worse
Occupations or activities that require repetitive forward bending (such as a nanny, a parent who carries small children, or someone who is involved in manual labor) may accelerate the progression of the slip over time. 6 Matz PG, Meagher RJ, Lamer T, et al. North American Spine Society. Clinical Guidelines for Multidisciplinary Spine Care. Diagnosis and Treatment of Degenerative Lumbar Spondylolisthesis. 2nd ed; 2016.
Who may need surgery for degenerative spondylolisthesis
Surgery for degenerative spondylolisthesis is rare. In general, patients with neurological symptoms, such as sensory changes or muscle weakness, who find little or no relief from nonsurgical treatments are more likely to benefit from surgery. 6 Matz PG, Meagher RJ, Lamer T, et al. North American Spine Society. Clinical Guidelines for Multidisciplinary Spine Care. Diagnosis and Treatment of Degenerative Lumbar Spondylolisthesis. 2nd ed; 2016.
Research indicates that 10% to 15% of individuals seeking treatment for degenerative spondylolisthesis eventually opt for surgical treatment. 4 Wang YXJ, Káplár Z, Deng M, Leung JCS. Lumbar degenerative spondylolisthesis epidemiology: A systematic review with a focus on gender-specific and age-specific prevalence. J Orthop Translat. 2016;11:39-52. Published 2016 Dec 1. doi:10.1016/j.jot.2016.11.001
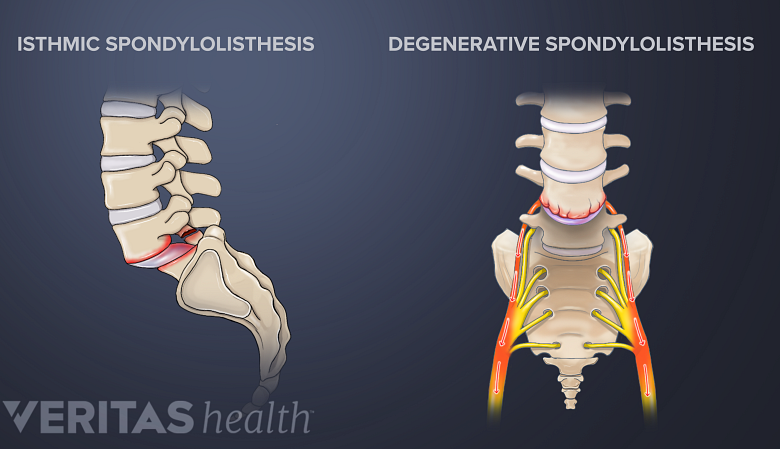
Degenerative Spondylolisthesis vs Isthmic Spondylolisthesis
Isthmic and degenerative spondylolisthesis are distinct conditions with similar symptoms.
It is important to note that a similar type of vertebral slip can also occur due to a structural defect in the small piece of bone, the pars interarticularis, which connects the two vertebrae on the back of the spine. This condition is called isthmic spondylolisthesis.
See Isthmic Spondylolisthesis Symptoms
Spondylolisthesis may also occur due to congenital, traumatic, or pathologic (related to bone disease) causes, but isthmic and degenerative causes are more common. 9 Jhaveri MD, Salzman KL, Ross JS, Moore KR, Osborn AG, Chang Yueh Ho. ExpertDDx : Brain and Spine. Philadelphia Elsevier; 2018.
While the symptoms of both these conditions may overlap, the underlying causes and risk factors are distinct.
When Degenerative Spondylolisthesis Is Serious
Degenerative spondylolisthesis is typically not a serious condition. The condition can become a medical emergency or require urgent care if it progresses to an extent that crucial spinal nerves are involved, or the stability of the affected segment is compromised.
In such cases, it is important to be able to identify the warning signs and symptoms of degenerative spondylolisthesis to ensure prompt medical attention and appropriate treatment.
Serious symptoms and signs are described below.
Progressive pain and weakness
It is important to seek immediate medical attention if there is persistent or worsening pain in the lower back that interferes with daily activities. The pain may radiate into the buttocks, thighs, or legs and may be accompanied by numbness, tingling, or muscle weakness. Additionally, any concerning progression of neurological symptoms, such as muscle weakness or loss of sensation should be evaluated by a physician urgently.
Changes in bowel or bladder function
Any changes in bowel or bladder function, such as difficulty controlling or emptying the bladder, bowel incontinence, or numbness in the genital area, is a medical emergency. These symptoms may indicate severe progression of spondylolisthesis leading to a serious condition known as cauda equina syndrome, which requires urgent surgical intervention. 4 Wang YXJ, Káplár Z, Deng M, Leung JCS. Lumbar degenerative spondylolisthesis epidemiology: A systematic review with a focus on gender-specific and age-specific prevalence. J Orthop Translat. 2016;11:39-52. Published 2016 Dec 1. doi:10.1016/j.jot.2016.11.001 , 7 Tenny S, Gillis CC. Spondylolisthesis. [Updated 2023 May 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430767/
See Cauda Equina Syndrome Symptoms
Significant loss of function or mobility
Functional disabilities, such as difficulty walking, maintaining balance, or performing basic movements, may indicate a more advanced stage of the condition that requires prompt medical intervention.
Any of these issues are potentially serious and warrant immediate medical attention.
See When Back Pain May Be a Medical Emergency
A specialist with advanced training in spine care can help evaluate and diagnose degenerative spondylolisthesis. Receiving personalized treatment at an early stage of the condition can help manage pain, prevent further complications, and enhance the overall quality of life for individuals with degenerative spondylolisthesis.
- 1 Akkawi I, Zmerly H. Degenerative Spondylolisthesis: A Narrative Review. Acta Biomed. 2022 Jan 19;92(6):e2021313. doi: 10.23750/abm.v92i6.10526. PMID: 35075090; PMCID: PMC8823594.
- 2 Cushnie D, Johnstone R, Urquhart JC, Gurr KR, Bailey SI, Bailey CS. Quality of Life and Slip Progression in Degenerative Spondylolisthesis Treated Nonoperatively. Spine (Phila Pa 1976). 2018;43(10):E574-E579. doi:10.1097/BRS.0000000000002429
- 3 García-Ramos CL, Valenzuela-González J, Baeza-Álvarez VB, Rosales-Olivarez LM, Alpizar-Aguirre A, Reyes-Sánchez A. Degenerative spondylolisthesis I: general principles. Acta Ortop Mex. 2020;34(5):324-328. doi:10.35366/97997
- 4 Wang YXJ, Káplár Z, Deng M, Leung JCS. Lumbar degenerative spondylolisthesis epidemiology: A systematic review with a focus on gender-specific and age-specific prevalence. J Orthop Translat. 2016;11:39-52. Published 2016 Dec 1. doi:10.1016/j.jot.2016.11.001
- 5 Bernard F, Mazerand E, Gallet C, Troude L, Fuentes S. History of degenerative spondylolisthesis: From anatomical description to surgical management. Neurochirurgie. 2019;65(2-3):75-82. doi:10.1016/j.neuchi.2019.03.006
- 6 Matz PG, Meagher RJ, Lamer T, et al. North American Spine Society. Clinical Guidelines for Multidisciplinary Spine Care. Diagnosis and Treatment of Degenerative Lumbar Spondylolisthesis. 2nd ed; 2016.
- 7 Tenny S, Gillis CC. Spondylolisthesis. [Updated 2023 May 22]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430767/
- 8 Samuel AM, Moore HG, Cunningham ME. Treatment for Degenerative Lumbar Spondylolisthesis: Current Concepts and New Evidence. Curr Rev Musculoskelet Med. 2017 Dec;10(4):521-529. doi: 10.1007/s12178-017-9442-3. PMID: 28994028; PMCID: PMC5685964.
- 9 Jhaveri MD, Salzman KL, Ross JS, Moore KR, Osborn AG, Chang Yueh Ho. ExpertDDx : Brain and Spine. Philadelphia Elsevier; 2018.