The goals of degenerative disc disease treatment are primarily to reduce baseline pain and prevent pain flare-ups as much as possible. Most cases of degenerative disc pain are manageable through a combination of pain management methods, exercise/physical therapy, and lifestyle modifications.
In This Article:
Pain Management
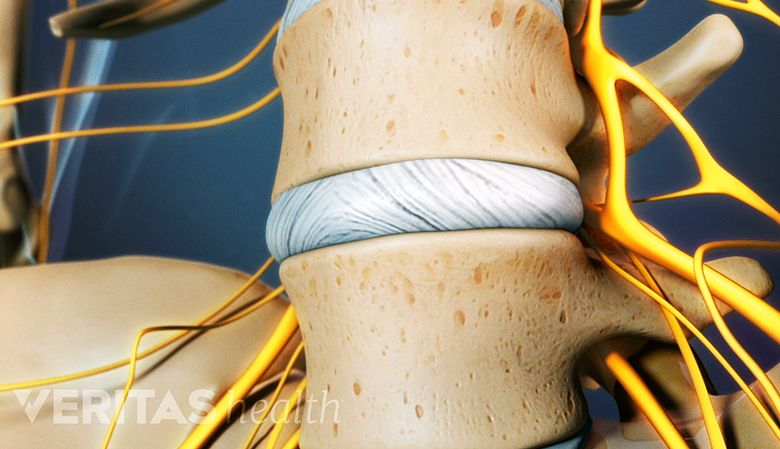
A key focus of pain management is to improve mobility and reduce pain so daily activities and rehabilitative exercise is more tolerable. Pain from a degenerated disc is usually attributed to instability, muscle tension, and inflammation, so these causes should be addressed.
Some pain management methods are administered at home as self-care practices, including:
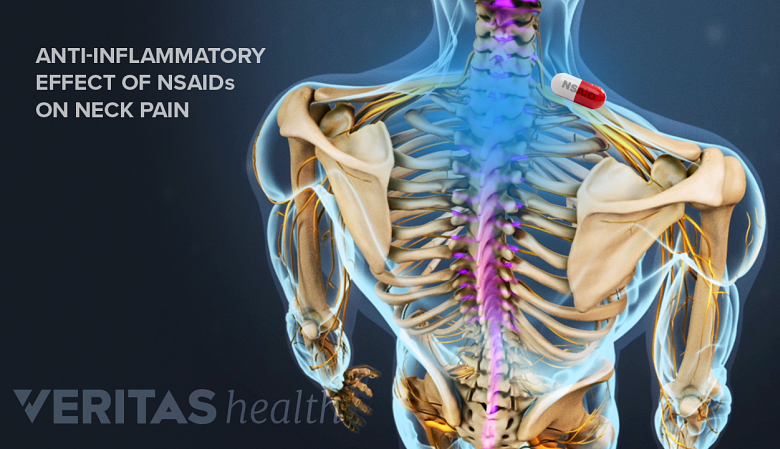
Pain medications
NSAID's have a calming effect on degenerative disc disease pain by reducing inflammation.
Over-the-counter pain medications fall into two main categories—pain relievers, such as acetaminophen (Tylenol), and anti-inflammatory medicines such as ibuprofen (Advil), aspirin (Bayer), and naproxen (Aleve). These medications are typically recommended for low-level chronic pain and mild pain episodes. For severe pain episodes, prescription painkillers such as muscle relaxants and narcotic painkillers may be recommended. Prescription pain medications are usually prescribed for short-term pain, as they can be highly addictive.
See Pain Medications for Degenerative Disc Disease Treatment
Ice or cold treatment
Applying ice or a cold pack to a painful area of the spine can relieve pain by reducing inflammation, which can be helpful following exercise or activity.
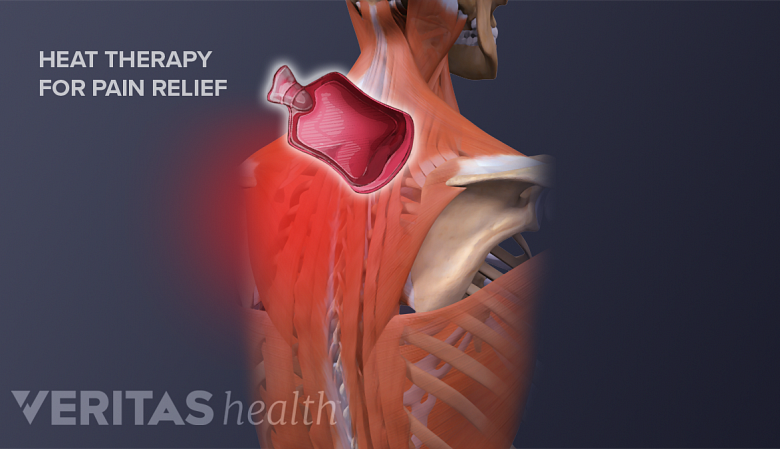
Heat therapy
Heat therapy fosters healing by improving blood flow.
Using heat from a heating pad, adhesive wrap, warm bath or other heat source can relax the surrounding muscles and reduce tension and spasms, a significant contributor to degenerative disc pain.
TENS units
A TENS unit (transcutaneous electrical nerve stimulation) is a small device that sends electric pulses through the body that interfere with and minimize pain signals. A TENS unit may include a device that transmits the signals directly over the skin, or a device that connects through wires to electrode pads worn on the skin, as well as a remote providing a range of frequencies for varying pain levels.
See Pain Management Techniques for Degenerative Disc Disease
Other pain management methods need to be administered by a qualified health professional, such as:
Manual manipulation
A chiropractor or spine specialist can manually adjust the spinal structures to relieve muscle tension, remove pressure from a nerve root, and relieve tension in the joints. Manual manipulation can provide temporary pain relief and improved mobility, and for some patients has been shown to be as effective as pain medications. 1 Healthy Quality Ontario. Artificial Discs for Lumbar and Cervical Degenerative Disc Disease –Update: An Evidence-Based Analysis. Ontario Health Technology Assessment Series. 2006;6(10):1-98.
See Manual Physical Therapy for Pain Relief
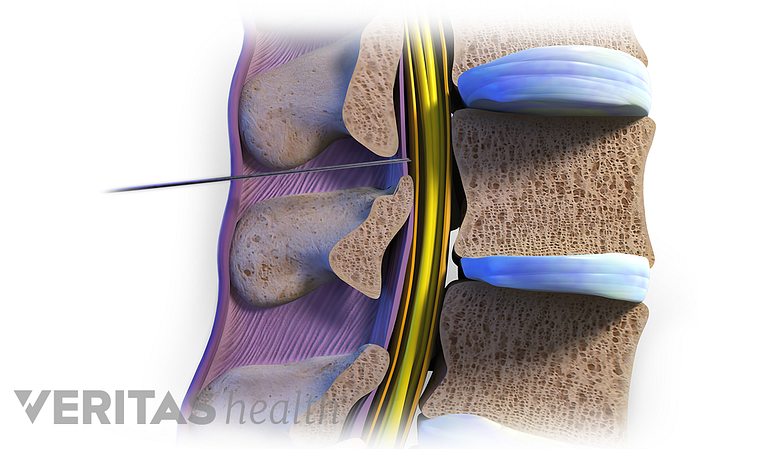
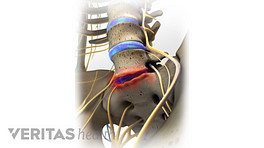
Epidural steroid injections
Epidural steroids reduce inflammation around compressed or impinged nerve roots in the spine.
A steroid injected around the spine’s protective outer layer can provide temporary pain relief, which helps to improve mobility. Injection treatments may be recommended prior to a physical therapy program, so exercises can be effectively completed with minimal pain.
See Epidural Steroid Injections
In many cases, trial-and-error is needed to find which types of treatment work best. Due to the long-term nature of degenerative disc disease, preferred pain management methods may change over time.
Exercise and Physical Therapy
Stretching helps reduce pain by relieving tension and building flexibility.
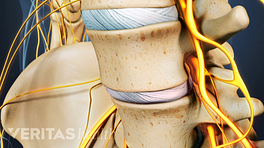
The goals of exercise are to help the spine heal and prevent or reduce further recurrences of pain. An exercise program for degenerative disc pain will typically include:
- Stretching. Targeted stretches are useful for decreasing tension and improving flexibility in the spinal muscles. For cervical disc pain, stretching muscles in the neck, shoulders, and upper back can relieve pain; stretching muscles in lower back, hips, pelvis, and the hamstring muscles can help alleviate low back pain.
- Strengthening exercises. Conditioning the muscles to better support the cervical or lumbar spine can help provide added support to a degenerating spinal segment, reducing pain and instability.
See Exercise and Physical Therapy for Disc Disease Treatment and Pain Management
- Aerobic exercise. Regular aerobic exercise is important for maintaining healthy circulation and keeping the joints and muscles active. Aerobic exercises elevate the heart rate, increasing the flow of nutrients and oxygen throughout the body, including to the spinal structures. Low-impact options are recommended for pain worsened by jostling or jolting motions, and may include a stationary bike, an elliptical machine, or water aerobics.
An additional benefit of exercise is that it can help reduce pain naturally, as it releases endorphins that serve as the body's natural pain reliever.
Exercises are best done in a controlled, progressive manner under the guidance of a physical therapist, physiatrist, chiropractor, or other appropriately trained healthcare professional.
Lifestyle Modifications
Staying hydrated helps keep discs healthy and functioning well.
Small, meaningful changes to daily routines can help improve overall health, which can in turn improve spine and muscle health. Some examples include:
- Avoiding nicotine
- Avoiding excess alcohol
- Drinking plenty of water
- Incorporating movement into a daily routine and avoid staying in one position for too long. For example, stand up to stretch and walk around every 20 to 30 minutes instead of sitting for a prolonged period.
- Use ergonomic furniture to support the spine, such as ergonomic desk chairs, a standing desk, or special neck pillows
See Food for Thought: Diet and Nutrition for a Healthy Back
The focus of this part of treatment is to provide education and resources that help develop a healthy lifestyle, minimizing stress on the spinal structures that can cause or contribute to pain.
- 1 Healthy Quality Ontario. Artificial Discs for Lumbar and Cervical Degenerative Disc Disease –Update: An Evidence-Based Analysis. Ontario Health Technology Assessment Series. 2006;6(10):1-98.