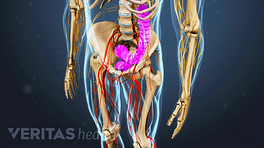
Cervical spondylosis with cervical myelopathy, commonly referred to as cervical spondylotic myelopathy (CSM), refers to impaired function of the spinal cord caused by degenerative changes of the discs and facet joints in the cervical spine (neck).
This condition is the most common disorder causing dysfunction of the spinal cord (known as myelopathy) and results from compression of the spinal cord.
Most patients with this condition are over 50 years of age, but the age of onset is variable depending on the degree of congenital spinal canal narrowing.
The process that leads to spinal cord compression is a result of arthritis in the neck (also called cervical spondylosis or degenerative joint disease), which is incompletely understood and likely has a number of causes.
In This Article:
Factors That Lead to Cervical Spondylosis with Myelopathy
Age-related changes in cervical vertebrae may contribute to cervical spondylosis.
Factors that are thought to contribute to development of cervical spondylosis with myelopathy include:
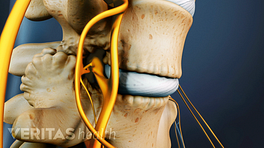
- Normal age-dependent changes of the intervertebral discs, most commonly manifested as cervical osteophytes (bone spurs) at the margins of the vertebrae
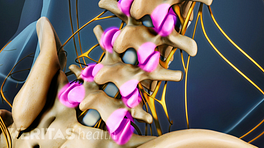
- Arthritis in the neck leading to facet hypertrophy (enlargement of the facet joints)
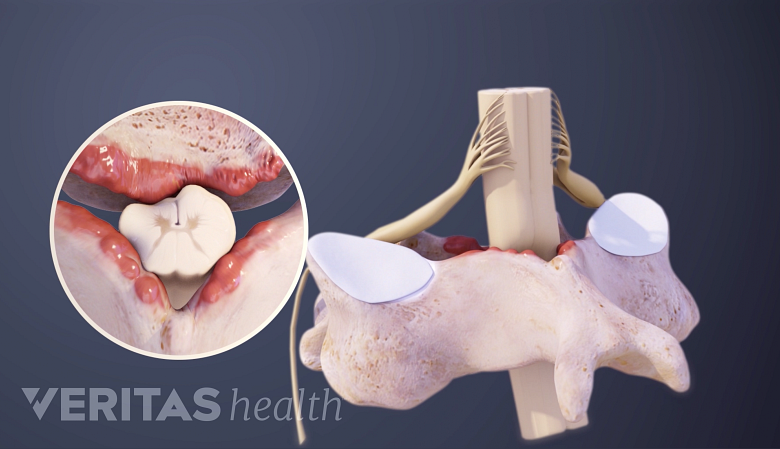
- Thickening of the ligaments surrounding the spinal canal, especially the ligamentum flavum, which parallels loss of disc height
- Translational mechanical instability resulting in subluxation (or partial dislocation) of the vertebral bodies
- Congenitally small spinal canal, which renders the patient's spinal cord more susceptible to compression
- Repetitive wear and/or trauma leading to degenerative changes affecting the disc spaces and vertebral endplates
These changes in the cervical spine produce narrowing of the spinal canal itself, leading to thickening of the posterior longitudinal ligament and bone spur (osteophyte) formation compressing the spinal cord, most commonly at the C4-C7 levels. The end result is chronic compression of the spinal cord and nerve roots leading to impaired blood flow and neurological deficit resulting in frank damage within the spinal cord itself.
A related condition that is more commonly being appreciated is ossification of the posterior longitudinal ligament (OPLL) that can also lead to chronic spinal cord compression.